Module 2: Breathing with
Why and how?
Deciding whether to have a tracheostomy is often quite a difficult task. The introduction to the chapter provides an overview of the most common situations when a tracheostomy might be needed. Normally, there will be plenty of time to make such a decision. It is best to gather information, discuss the matter with those experienced in such treatment and make the right decision with those in charge of the treatment. A tracheostomy can then be planned. Sometimes a tracheostomy might be done due to an acute disease when invasive mechanical ventilation therapy is necessary in an emergency situation. The objective is to establish open airways, prevent infections, remove mucus and reduce the risk of chronic infection in the lungs.
Observation
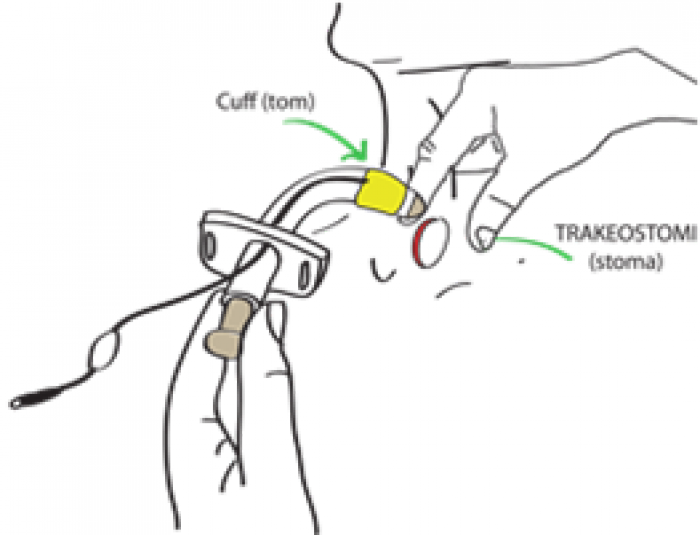
Initially, after tracheostomy is performed it is important to observe whether bleeding from the stoma (hole in the throat), swelling or pain occurs. This may be quite normal. Once the stoma is stable, usually within 2 weeks, a tracheostomy tube change may be performed. It is necessary to look out for any signs of infection, such as sores, pus, swelling, granulation tissue, increased amount of mucus, and whether the cannula is positioned correctly in the throat and that the tracheostomy tape is comfortably tight.
Complications
Acute complications associated with a tracheostomy are rare Severe haemorrhaging or air leakage to the area between the lungs and walls of the chest or the area between the lungs or subcutaneous tissue can occur, therefore careful monitoring is performed in the immediate postoperative period after the tracheostomy. Problems or complications that could arise later:
Leakage around the opening (the stoma, is indicated by the expulsion of secretions, air leakage during ventilation or an impaired voice. If these complaints are severe or persistent, the cannula can be replaced with a larger size.
Infection around the stoma opening
Redness, pus, swelling and occasional pain around the opening of the stoma could indicate an infection. This is usually treated locally.
Infection in the airways/lungs
The general feeling of unwellness, fever, elevated cough, breathlessness, pain, blood in the mucus or changed volume, colour or consistency of the mucus can all indicate infection and must normally be treated with antibiotics. More effort must also be applied to clearing secretions.
Formation of scar tissue, granulated tissue
- Granulation tissue can form around the opening of the stoma. This can lead to pain when changing the cannula, minor bleeding and discomfort. It is normally treated locally with silver nitrate sticks and by preventing cannula chafing.
- Granulation tissue can form at the tip of the cannula inside the trachea. It can cause bleeding and problems when changing the cannula and, in some cases, make mechanical ventilation difficult. In general, the doctor will examine with a fibre-optic camera (bronchoscopy) to look for this type of problem on suspicion. If present, the cannula will normally be changed and adjusted to prevent chafing in the same area. Surgical treatment is rarely necessary.
Miscellaneous
- Sores in the trachea from suction damage can give minor bleeding. Too much air or liquid in the cuff can expand the trachea or lead to a narrowing (stenosis). This is best prevented by adequate cuff maintenance routines.
Acute adverse events can occur with a tracheostomy. Read more about this under Acute adverse events.
Changing cannulas and inner cannulas
Tracheostomy care routines aim to maintain the size of the stoma, prevent skin irritation and infection, reduce the risk of infection in the airways and to prevent mucus from blocking the cannula. If you have a tracheostomy, it is important that those who will be helping you are given adequate training on caring for a stoma and the cleaning of an inner cannula (if applicable). Generally, a doctor or specially trained personnel will change/replace a cannula once per month/every 30 days at an outpatient clinic or in your own home.
With a tracheostomy, you are more exposed to infection. Therefore, good hygiene is important to prevent infection.
The skin around the cannula and the inner cannula (if applicable) is washed twice per day or more often, as required. You and those helping you must also be trained in the following:
- Caring for a tracheostomy.
- How to clean a cannula and inner cannula.
- How to use suction and suction techniques.
- How to change a cannula.
- How to use a Lærdals bag (resuscitator).
You can find an example of tracheostomy procedures here (external page).