Traveling inland
We recommend that you make a list of equipment that you need on travels when you need comprehensive breathing aid. Particularly important for flights.
Checklist
Booking of ticket. The flight ticket is booked in advance with the local travel company, or you can call the airline directly and order it there. Airlines have fixed procedures for how they can help - and they know the different airports.
What types of information is important to provide? First of all you should inform that you have a disability that means that you need assistance at the gate, to get out to the plane, in the cabin, and that you otherwise need special facilities. If possible, your needs will be taken into account. You will be notified when you book the ticket if your wishes can be met. An example of such information may be:
- That you depend on a wheelchair
- That you use an electric wheelchair
- That you need assistance for luggage
- That you need assistance out to the plane
- That you need assistance all the way to your seat
- That you need to board before other passengers
- That you need assistance on board the plane
- That you are using a ventilator
- If you use portable oxygen equipment, ask your supplier to check if it is permitted to be used on board an aircraft.
Do you have technical aids or electronic equipment you rely on? Electronic equipment radiating electromagnetic energy must not be used aboard the aircraft, as this may affect the electronic airplane systems. If you use technical aids such as a wheelchair, there may be limitations in size, weight and number of wheelchairs included in each flight. If you are using BiPAP or ventilator, you should inquire if you can bring and use this in the cabin or if it is to be sent as a luggage. All modern ventilators approved for life-sustaining treatment are also approved in accordance with the radiation requirement, but the airline may require documentation.
Do you have heart or lung disease? The air on board aircrafts is continually shifted, so even with full airplanes and many people on board there should always be a good indoor climate. On larger aircraft there is also oxygen on board. This oxygen is meant to be used for emergency situations. If you know that you will need oxygen during the flight it is important that you give the airline information about this in good time.
Do you use medical oxygen? If you need to use oxygen during the flight, it is important that you give the airline notice in good time. Some airlines will accept that you include oxygen cylinders approved for use in airplanes, while others require you to use their oxygen bottles during the trip.
The agreement with the airline must be made no later than 48 hours before departure. It is always better nevertheless that such a deal is made when booking the trip. You need to clarify that you need gas bottles with regulator, so you get exactly the dose you need. The bottles are delivered at check-in at the departure point, or they will be pre-assembled on board flights, as it is done for example with SAS (airline). Please note that it is not permitted to use liquid oxygen on airplanes. If you want to use such oxygen at your destination, you will normally be allowed to bring empty containers as checked baggage. For further information, please contact your supplier.
Do you need an assistant? Some airlines offer reduced rates for a necessary companion or assistant. This requires medical confirmation. Do you need medical assistance during the flight? The airline can not take responsibility for providing you with medical treatment or care during a flight. Nor can they give you special medicines that you cannot take for yourself. If you need this type of medical assistance, your journey must be classified as a medical transport. There are special routines for medical transport.
- Check out show times in advance
- Calculate good time
- Inform about your needs
- Are you unsure, just ASK
- Remember, you are a customer!
On board the plane. Provide information to cabin staff about what you think they should know. Find or ask for a space at the aisle, so you will get easier contact with the flight crew when you need help or if you have any questions.
Mobility impaired. For the flight itself, some provisions apply by international and national authorities. They include flight safety and routines in case of emergencies. The rules do not include disabled people as a group, but make demands on people with disabilities. This means that you can not sit on the seat at an emergency exit. For those who are mobility impaired, the flight can be somewhat uncomfortable. If your wheelchair is equipped with a seat cushion, you can use it in the airplane as long as it does not prevent the use of a safety belt. Then you are more comfortable and steady. There are also pillows and blankets on board that can give you support.
Toilet visits can be difficult for disabled people on flights. Work is being done to develop transport chairs that will make the situation easier for some users. Some new aircrafts are now being built with a larger toilet. These are in front in the aircraft.
Travelling abroad
All technical respiratory equipment that is used in Norway is permanently borrowed and belongs to the hospital unit for assistive devices. In the event of technical faults or breakdowns, the unit is responsible for servicing and providing replacement devices. However, such responsibility is limited to domestic travel. Therefore, it is crucial to plan well when travelling abroad. For safety reasons, the specialist in charge should be consulted to discuss which additional equipment is required. A spare ventilator should always be taken along, as it could be fatal or health damaging if the ventilator breaks down. In some cases, it might be relevant to borrow an extra machine. A list of resource persons and organisations in various countries is available on the American web site of the International ventilator Users Network , which can be downloaded as a pdf.


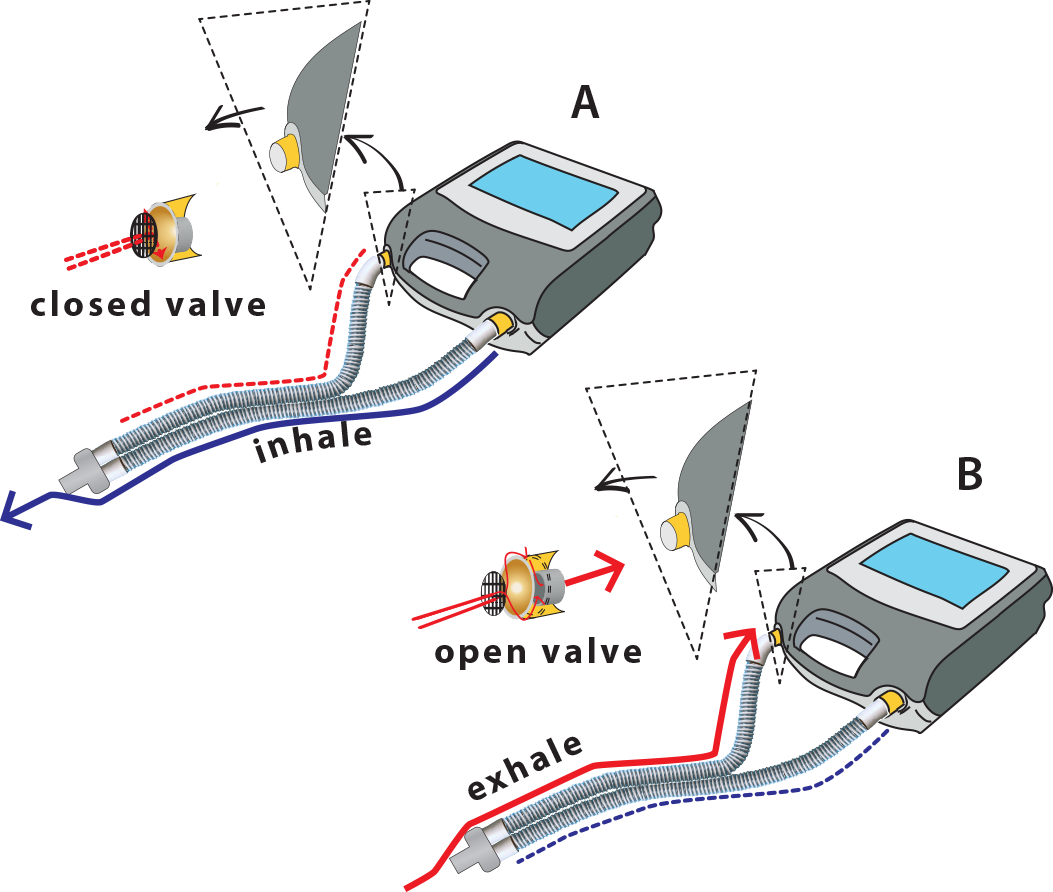
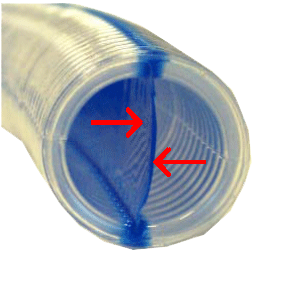
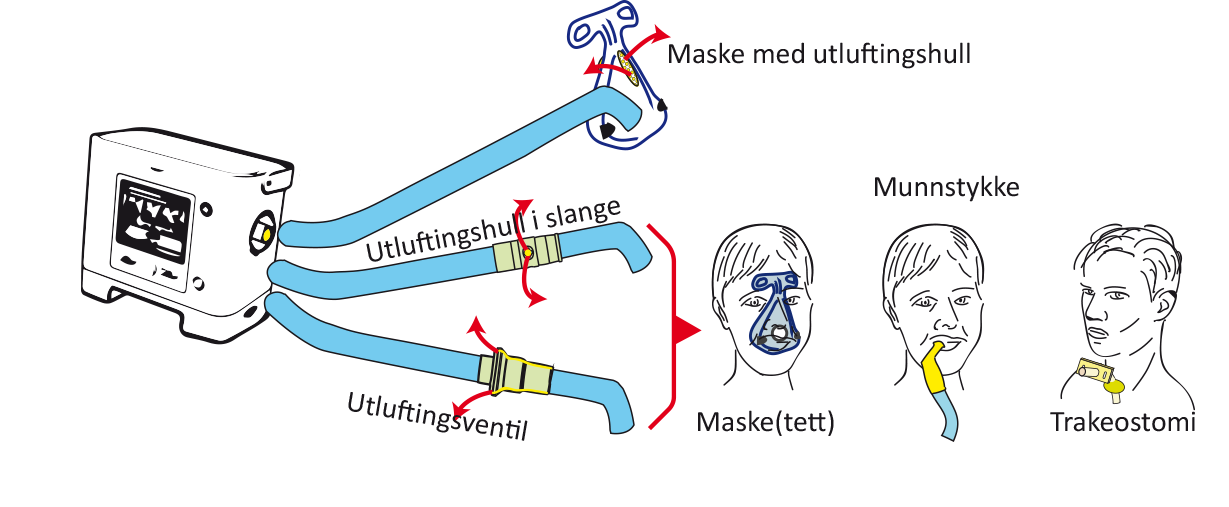
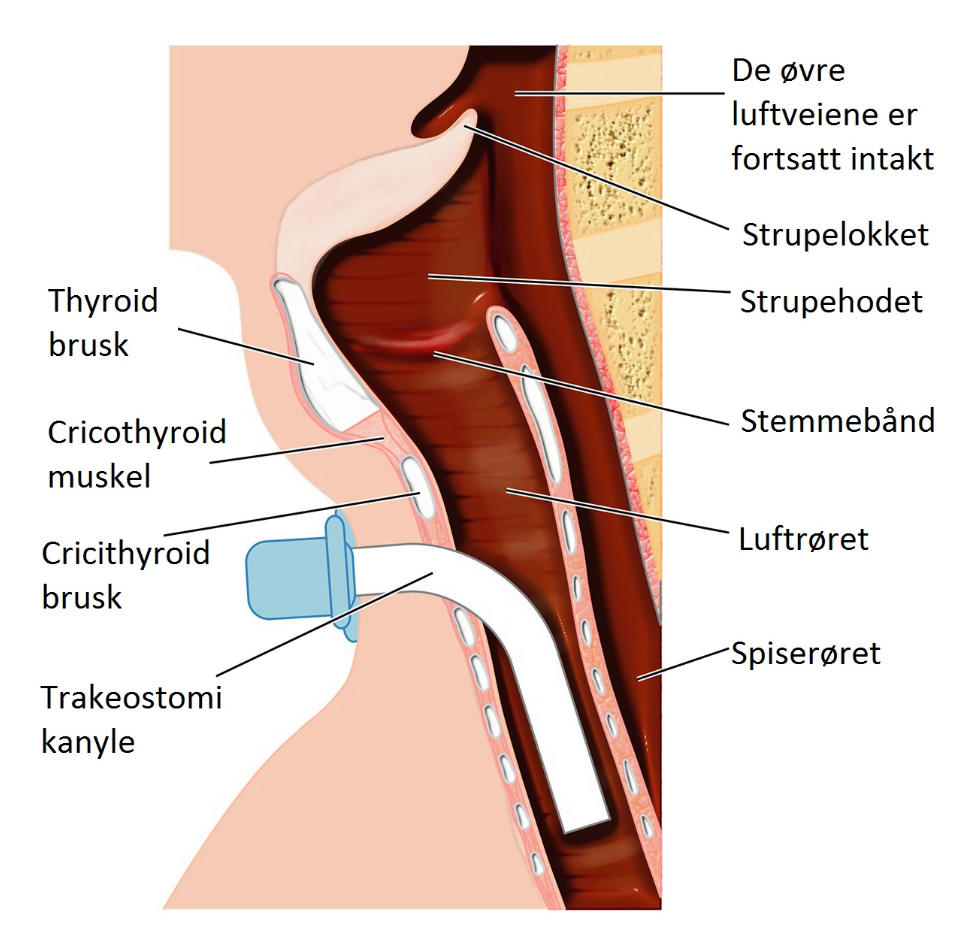
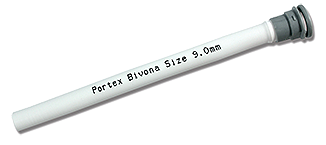
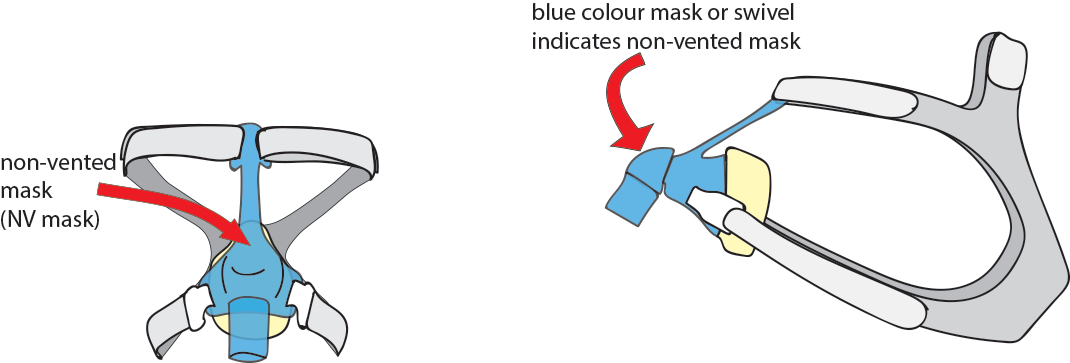
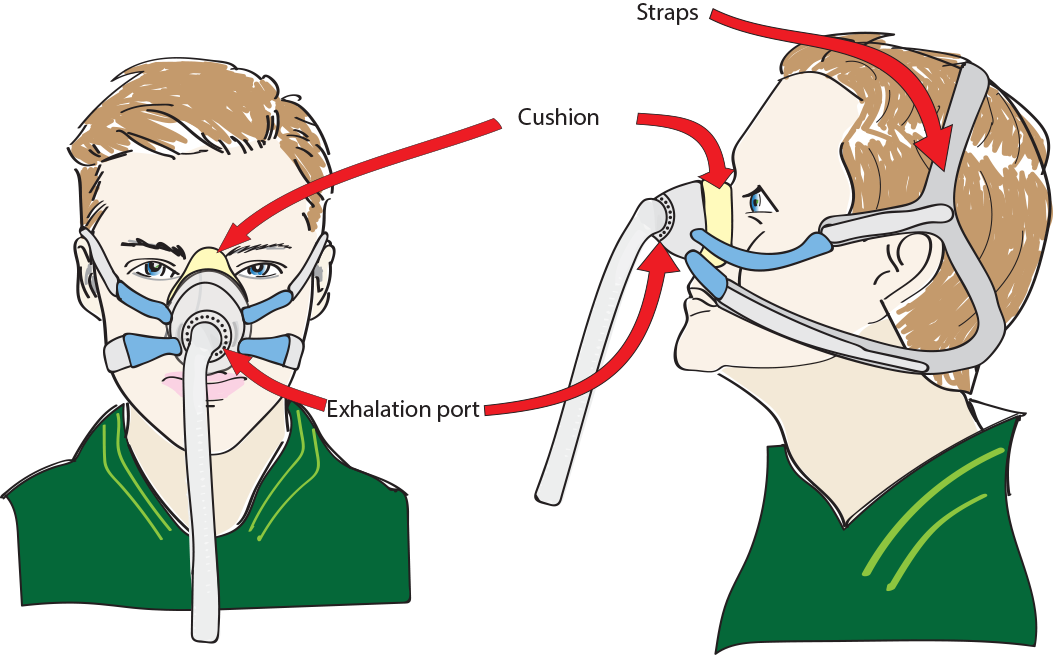
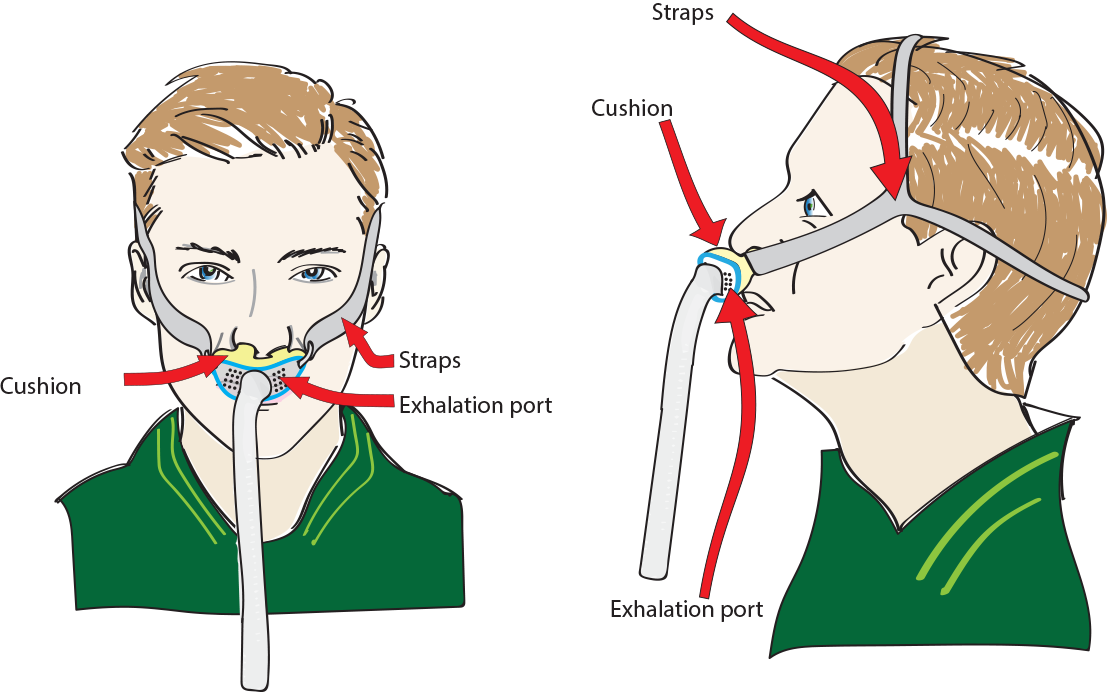
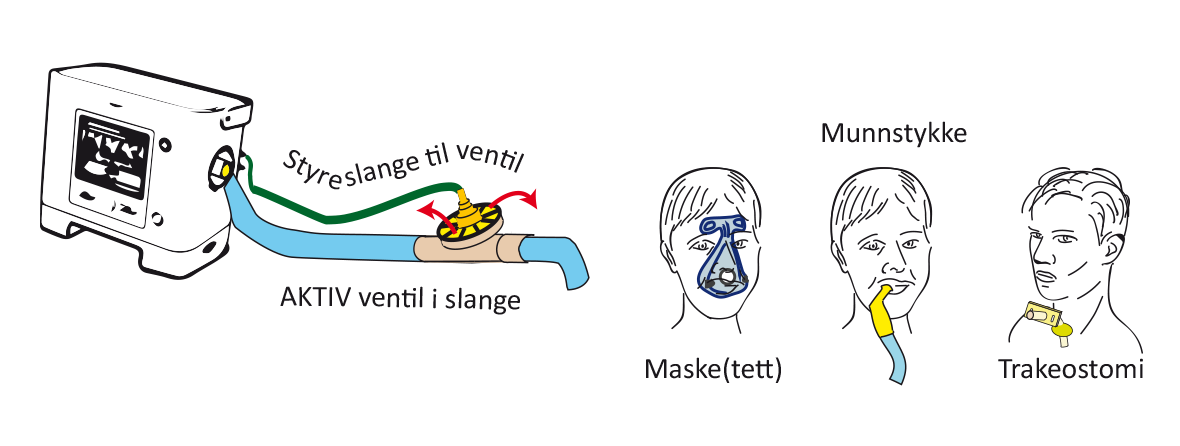 Ventilator with active valve circuit and simple hose.
Ventilator with active valve circuit and simple hose.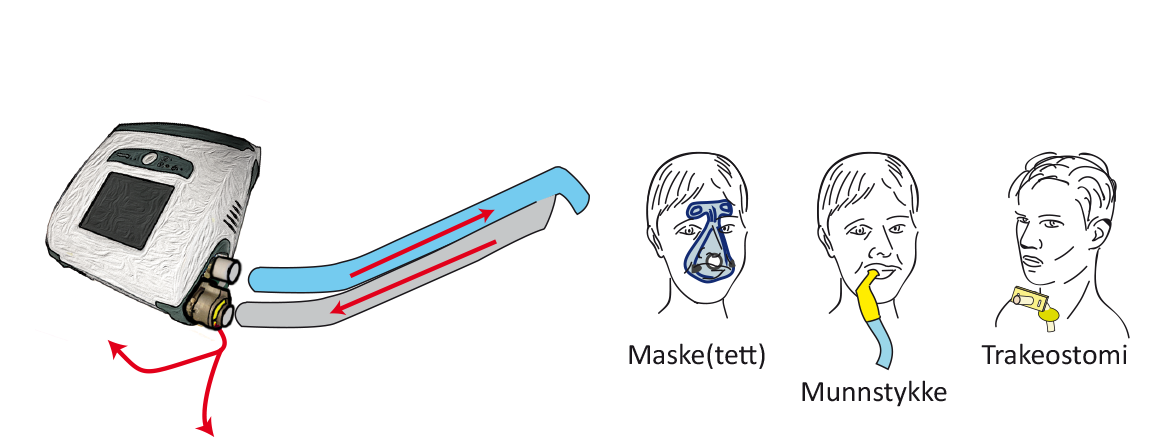
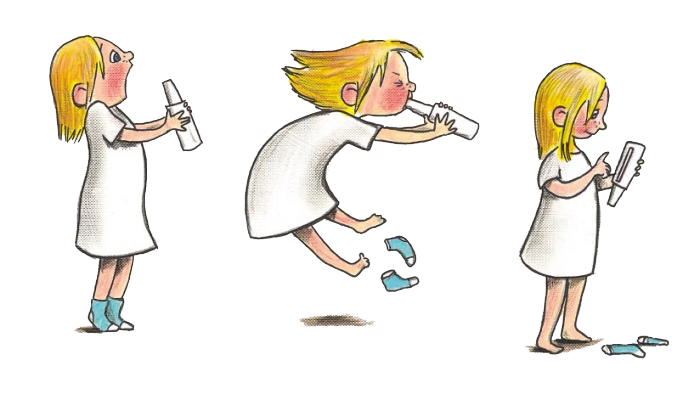





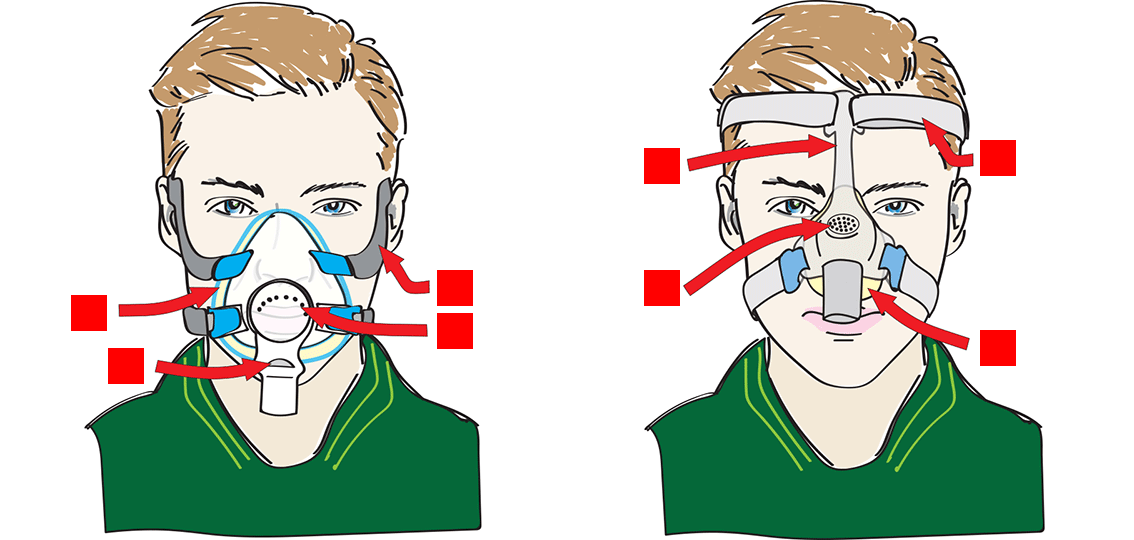

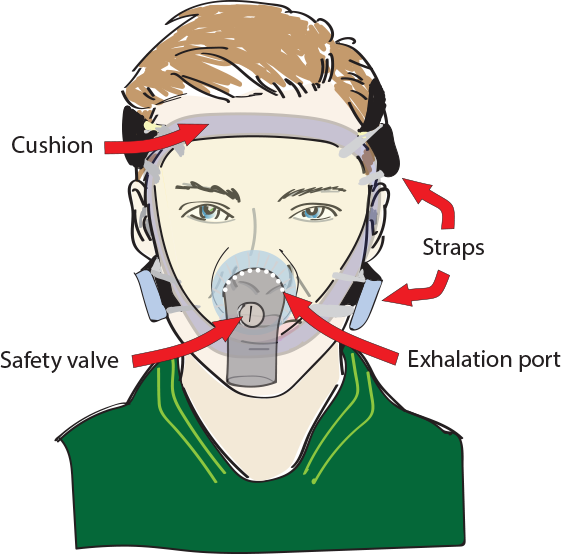
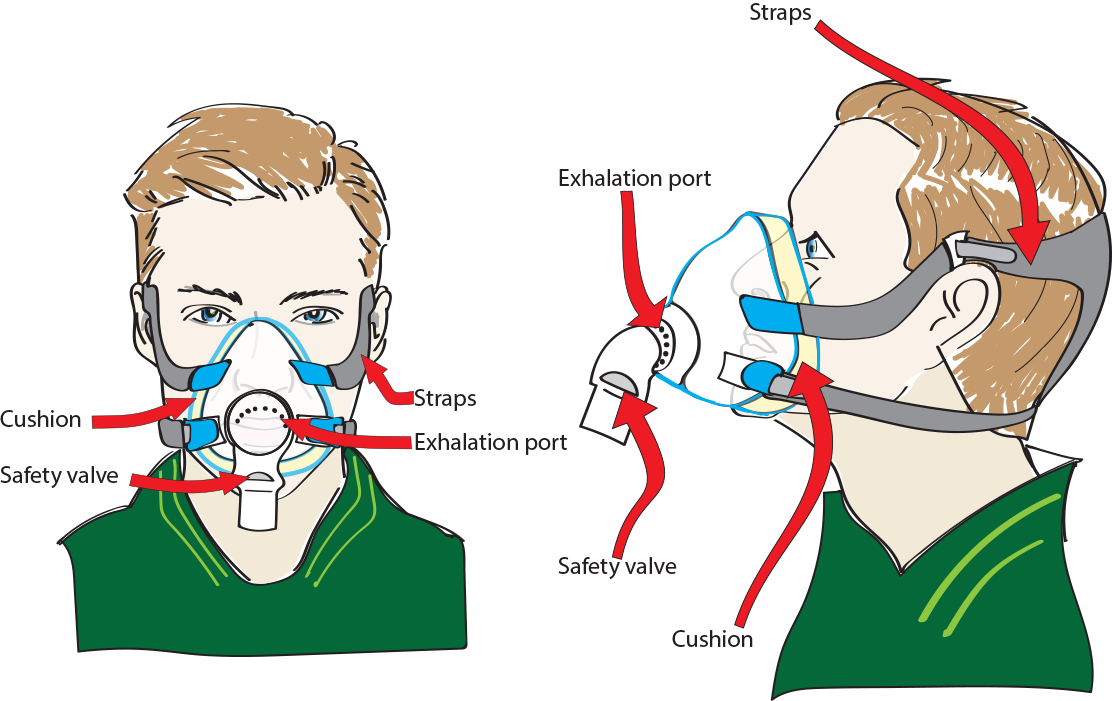 Oronasl mask
Oronasl mask