Module 2: Breathing with
Breathing equipment
Ventilators
A life-sustaining ventilator ("respirator") differs from a BiPAP machine primarily because it is also approved for usage when one is completely dependent on a machine to stay alive. It must have an in-built battery in case of power failure and a full range of alarms. Due to battery they are suitable for use during transportation. They also durable and withstand severe physical blows, for example, falling off a table or a wheelchair.

Patients with a tracheostomy will always need asuch advanced ventilators, but even in nonivasive (ie mask or mouth piece) ventilation, users may need the flexibility and security provided by a "respirator". The breathing circuit, i.e. the hose from the ventilator to the user, may be similar to that of a BiPAP machine, but a more advanced valve is often used to control the shift of ventilation from inspiratory to expiratory phase.
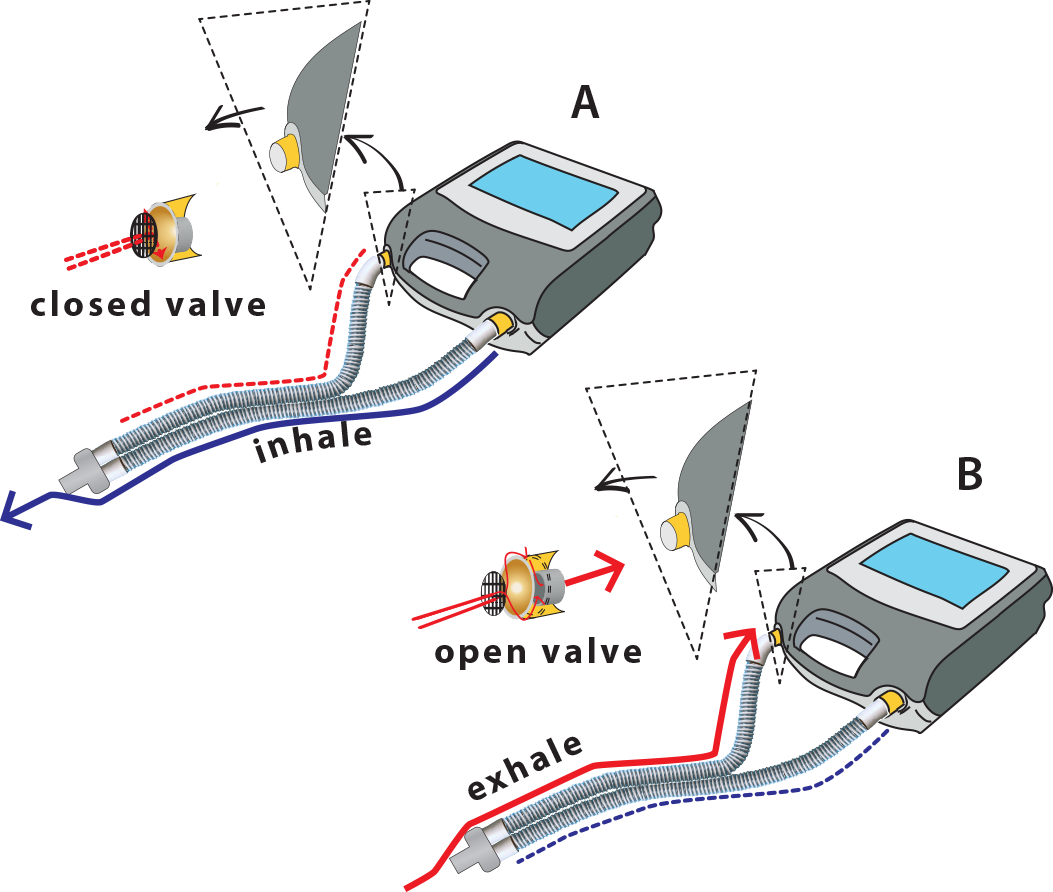
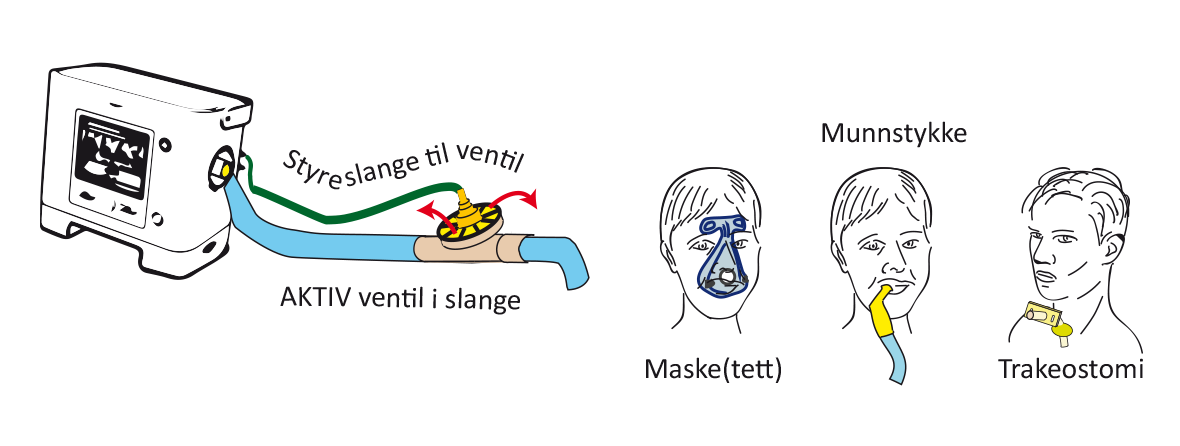
Illustration of how a ventilator valve can be placed on the ventilator hose itself. We also see how a balloon on the valve grows bigger and closes a hole during inhale, while the balloon empties during exhale.
As the figure illustrates, the valve can be an integrated part of the hose and situated close the the user. These types of valves have a balloon or membrane, which blows up or moves to close a hole in the valve, allowing air to dissipate during opening, ie exhalation. In some machines, the valve is built into the ventilator itself. The expired air must be returned to the ventilator before it is expelled in such cases. In order to achieve this, two hoses must be attached to the ventilator, one for inspiration and one for expiration. This is called a dual-limb circuit.
Double circuit active valve
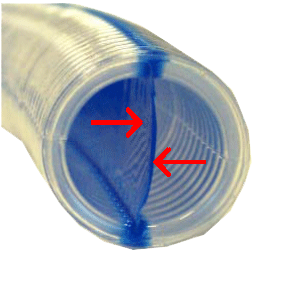
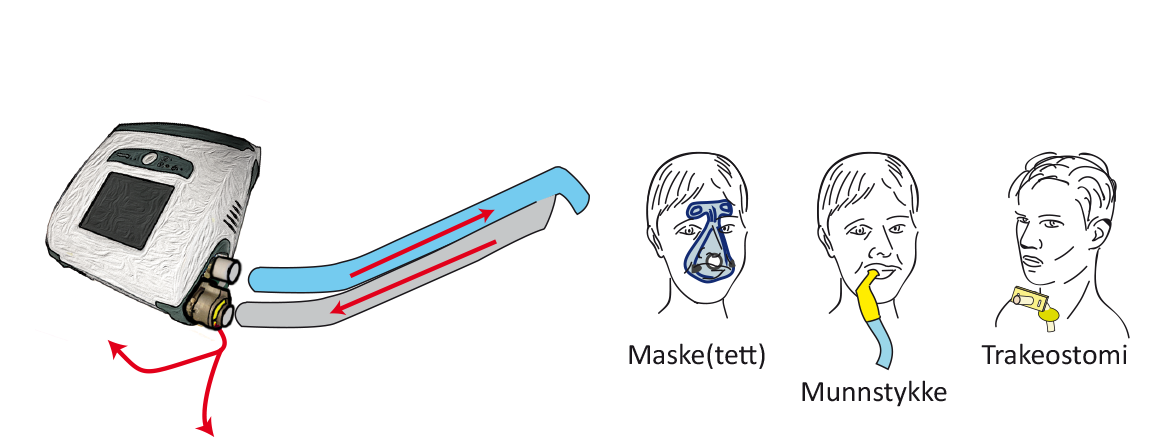
A dual limb circuit may be contained in a single hose with a split membrane, effectively dividing the hose in two separate parts. In one part fresh air from the ventilator passes through the patient and in the other part used air flows back to the ventilator with its valve. Limb-O circuit is such a ventilator tube with a dual-limb circuit in a single hose. See fig.
Most ventilators for home care provided in Norway can also be used without an integrated or active valve in the circuit. In these cases, the ventilator is working like a BiPAP device and exhalation occurs passively through a hole in the mask or the circuit itself. Ventilators with these capabilities may be coined hybrid ventilators, is, capable of performing like a BiPAP device or a "respirator". The advantage of using a BiPAP circuit instead of an active valve is that it is more simple and easy to maintain. The disadvantage is that more air continually flows through the ventilator hose, which could be a problem in terms of humidification. In addition, the ventilator must ‘work slightly harder’ to compensate for a higher leakage of air, which means that the operational lifetime of the internal battery is going to be shorter.
I
Connection
Connection sequence: Power supply → ventilator → ventilator circuit → connection (mask, mouthpiece or tracheostomy).
As mentioned, the ventilator circuit can be single or dual, and it can include a valve controlling inspiration and expiration (active valve) or just an open hole in the tube or mask where expired air can leak out (passive valve).
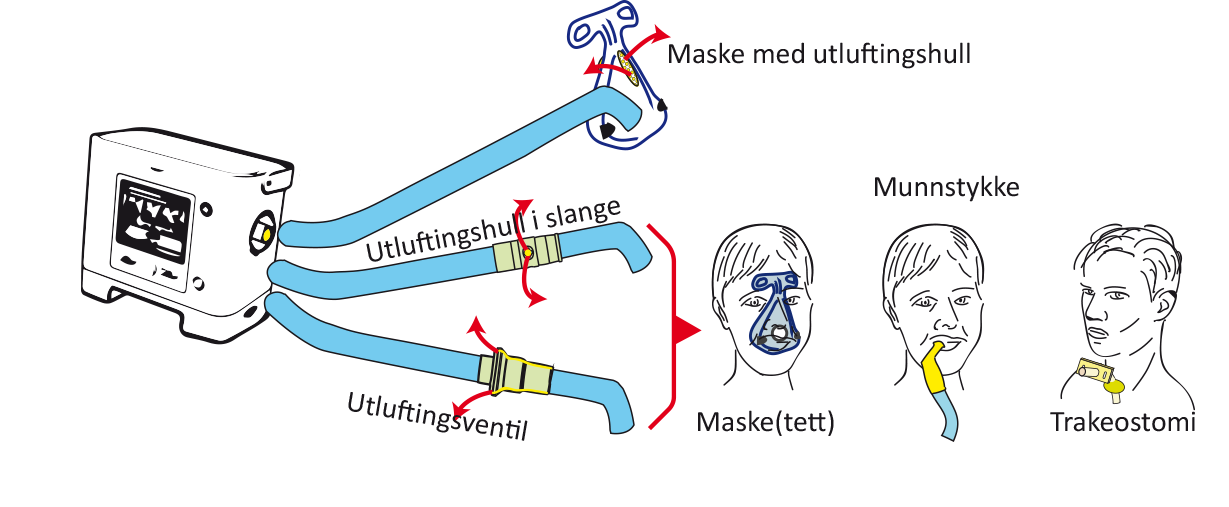
Ventilator with passive valve circuit and simple hose.
 Ventilator with active valve circuit and simple hose.
Ventilator with active valve circuit and simple hose.
On and off
The start button normally only has to be pressed once to start a ventilator (e.g. Trilogy). Sometimes the machine has a standby feature. These machines have a separate main switch, which must be pressed first (e.g. Elisee, Astral, PB560, Vivo 50/60).
Turning off a ventilator always entails a two-step process. Generally, the on/off button must be pressed and then the user will be need to confirm that the machine is to be turned off by either pressing another button (Trilogy, Elisee, Astral) or repressing the on/off button.
Example of how to turn a ventilator on – Trilogy:
- Press the on/off button.
- Click 'Yes' to confirm.
Alarms
Modern ventilators have numerous alarm options available. What type and how many alarms are activated will depend on the individual patient, e.g. based on his/her breathing reserve. When the therapy is life supporting, immediate assistance is required in case of emergency. Typically, it can take up to 15 seconds for an alarm to sound and it must be possible to solve the problem within one minute. Ventilator alarms are a combination of sounds, light and text in a ventilator display. Every machine is different in this regard, but they are able to react to the same adverse events in general. Critical alarms and medium or low-priority alarms are differentiated.
Important alarm categories:
- Alarms indicating low ventilation of the patient may be cause by:
- leakage/disconnection (critical)
- blockage (critical)
- Power supply alarms may sound because:
- the ventilator has shifted from a mains voltage to internal battery supply (low-priority alarm)
- the battery is about to go flat (critical)
- Technical alarms:
- Faulty machine or filter (often critical)
Cleaning
- Ventilator - general dusting
- Air filter - clean regularly (every two-four weeks) and replace every six months.
- Valve - clean regularly. Every two weeks for those with a tracheostomy.
- Tube - clean or replace. Every two weeks for those with a tracheostomy.
- Miscellaneous: See Special considerations, using checklists below
Humidification
Tracheostomy patients receive air from the ventilator directly into the air tube (trachea). Therefore, it is an advantage if the air has been humidified and warmed up, as it no longer passes through the nose. It can be humidified and warmed up in the following two ways:
- Passive humidification: Via a heat and moisture exchange filter, a so-called ‘artificial nose’. The patient’s expired air passes through the filter, and a small amount of the heat and moisture in the expired air remains in the filter. Some of the heat and moisture in the filter will then be used when the next aspiration starts.
- Advantages: Easy. The only alternative for wheelchair users in the absence of electricity.
- Disadvantages: May be insufficient and lead to stickier mucus.
- Active humidification: Heating plate with a humidification chamber that vaporises air. Temperature sensors that register the temperature of the humidification chamber and the temperature close to the patient regulates the temperature of the heating plate. The ventilator tube has heating wires that prevent condensation.
- Advantages: Gives the best heat and moisture.
- Disadvantages: Complicated tubing system. Requires electricity from the mains supply.
Carrying out checks/follow-up
Hospital outpatient clinics follow-up ventilator patients and in some cases home visits are made. Ventilator settings rarely have to be adjusted for tracheostomy patients with life-sustaining treatment or those with a stable disease. Ventilator settings and the methods used to obtain the best ventilation might significantly change in line with the progression of the disease if a patient has a disease that gradually changes. Check-ups are mainly carried out at hospital outpatient clinics or departments, but home visits are also useful and in many cases necessary. The interval between specialist check-ups varies and is typically between three to six months. In rare cases, annual check-ups suffice.
Challenges
Home mechanical ventilators are often adjusted in the homes of users who have had breathing problems for a some time and have experience with simpler BiPAP therapy. The main challenge is usually in finding adequate methods that allow respiratory support to be given at various times within a 24-hour period or in different situations, e.g. during the night and day whilst sitting in a wheelchair. Sometimes it is advantageous to have different masks or alternate with a mask during the night and mouthpiece during the day. In order to do this, the ventilator must normally have various settings and tubing circuit.
Special considerations
Safety
Due to the alarms, users or assistants/relatives must always understand the information and act accordingly (see the section on alarms above). Patients who require practically around the clock respiratory support always have two machines. Many users have two machines for practical reasons, e.g. they need respiratory support whilst in a wheelchair or because they need some active humidification during a 24-hour period, but can otherwise manage without.
Checklists
The National Advisory Unit on longterm machanical ventilation (NKH) has prepared a number of proposals for checklists that could be of practical help to patients with home mechanical ventilation and their daily living.
Diseases
Various problems can arise in connection with the administration of effective ventilator therapy with the presence of respiratory infections, colds, bronchitis or pneumonia. In general, it is most important to have adequate methods for clearing mucus (see the relevant chapter). In some cases, it might be beneficial to change from a nose to mouth/nose mask. Tracheostomy patients might require more humidification.